Fracture Blisters: Symptoms, Causes, and Treatment Options
Imagine you’re in the emergency room, your ankle throbbing after a bad fall. The doctor confirms it: you’ve broken a bone. But then, a few days later, you notice something strange—blisters forming on your skin, right over the fracture site. You’re confused, maybe even a little worried. What are these blisters, and why are they there?
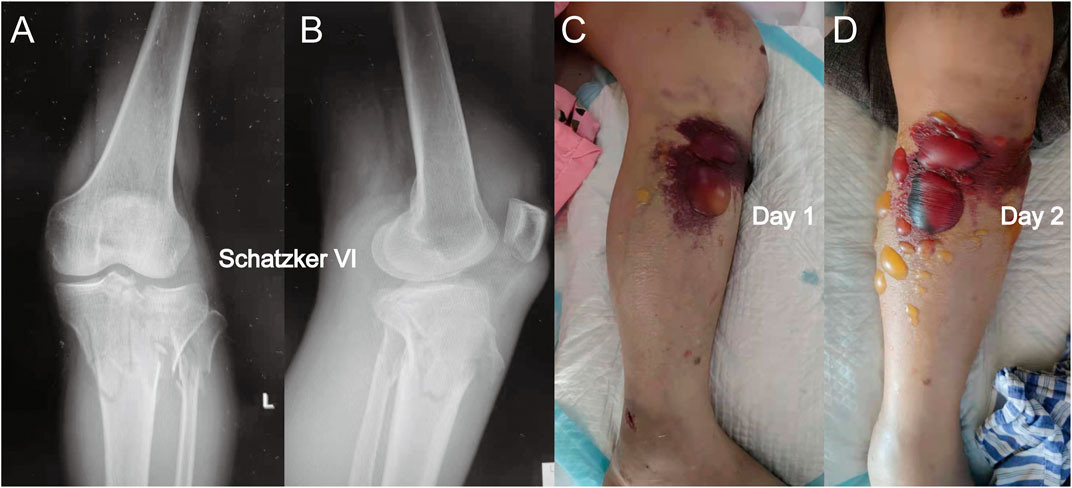
(A Proximal Leg Fracture with Fracture Blister developed over it)
What Are Fracture Blisters?
Fracture blisters are fluid-filled vesicles or bullae that
form on the skin overlying a fractured bone. They are a sign of significant
soft-tissue injury and occur in approximately 2.9% of all fractures requiring
hospitalization (Verywell Health). These blisters are most commonly seen in
areas where the skin adheres tightly to the bone with little subcutaneous fat,
such as the ankle, wrist, elbow, foot, and distal tibia. They resemble
second-degree burns in appearance but are caused by mechanical trauma rather
than heat.
Fracture blisters can be single or multiple and may appear
directly over the fracture or at a distance, depending on the injury’s impact
on surrounding tissues. They are more likely to occur in high-energy injuries,
such as motor vehicle accidents or falls from significant heights, but can also
develop in low-energy trauma, like a moderate ankle sprain, in up to 25% of
cases.
Pathophysiology: How Do Fracture Blisters Form?
The exact cause of fracture blisters remains partially
elusive, but research suggests that damage to the dermal-epidermal junction—the
interface between the skin’s outer (epidermis) and inner (dermis) layers—plays
a central role. When a bone fractures, particularly with significant force, the
skin experiences shearing stresses that can separate these layers, creating a
potential space for fluid accumulation.
A 1995 biomechanical study by Giordano et al. demonstrated
that the tension induced by fracture deformation causes this dermal-epidermal
separation in cadaveric ankle skin specimens. The study highlighted that the
differing elasticity and viscoelastic properties of the dermis and epidermis
lead to layer splitting when critical strain is reached. Post-traumatic edema
(swelling) increases interstitial pressure, reducing cohesion between epidermal
cells and promoting fluid transfer into the blister cavity (PMC Article).
Additionally, damage to local blood vessels and lymphatics
contributes to venous stasis and tissue hypoxia, which can lead to epidermal
necrosis. This combination of mechanical stress, swelling, and reduced oxygen
supply creates the perfect storm for blister formation. Histologically, a 1993
study by Varela et al. confirmed a typical dermo-epidermal junction split with
re-epithelialization, noting that intact blisters are sterile but become
colonized with pathogens like Staphylococcus aureus and Staphylococcus
epidermidis upon rupture.
Types of Fracture Blisters
Fracture blisters are classified into two clinical and
histological types:
|
Type |
Location of Cleavage |
Characteristics |
Healing Time |
Complications |
|
Clear Fluid-Filled (Subcorneal) |
Within the epidermis, above the granular layer |
Contains clear, gel-like serum; minimal dermal damage;
heals without scarring |
~13 days |
Lower risk |
|
Blood-Filled (Subepidermal) |
Between epidermis and dermis |
Contains blood from damaged papillary dermal vasculature;
may scar or alter pigmentation |
~16 days |
Higher risk |
Both types indicate a cleavage injury at the
dermal-epidermal interface, but blood-filled blisters are associated with more
severe tissue disruption, increasing the likelihood of complications like
infection or wound dehiscence.
Where and When Do Fracture Blisters Occur?
Fracture blisters are most frequently observed over
fractures of the ankle and proximal tibia, followed by the wrist, elbow, and
foot. These areas are prone due to their thin skin, minimal subcutaneous fat,
and lack of cushioning muscle or tissue. For example, the ankle has few hair
follicles, sweat glands, or deep veins, making the skin particularly vulnerable
(DermNet NZ).
Timing is variable:
- Typical
Onset: 24–48 hours post-injury, with an average of 2.5 days.
- Range:
As early as 6 hours or as late as three weeks.
- Post-Surgical:
Can occur after elective foot and ankle surgery.
Blisters may not always form directly over the fracture
site; they can appear at a distance due to the injury’s broader impact on soft
tissues. Curiously, areas like the wrist, elbow, and foot, despite having
similar skin characteristics, are less commonly affected, possibly due to
differences in injury patterns or tissue dynamics.
Risk Factors
Fracture blisters are more likely in:
- High-Energy
Injuries: Falls from heights (~18 feet), motor vehicle accidents, or
Gustilo Anderson Grade I/II open tibia fractures.
- Low-Energy
Trauma: Up to 25% of cases, such as ankle sprains or moderate blunt
trauma.
- Predisposing
Conditions: Diabetes mellitus, peripheral vascular disease, collagen
vascular disease, hypertension, smoking, alcoholism, and lymphatic
obstruction, all of which impair wound healing.
Notably, age, sex, race, overall health status, concurrent
injuries, or initial fracture treatment do not appear to influence blister
formation.
Diagnosing Fracture Blisters
Diagnosis is primarily clinical, based on the appearance of
tense, fluid-filled vesicles or bullae on swollen skin overlying a fracture.
Healthcare providers should document:
- Number
of blisters
- Location
- Size
- Type
(clear or blood-filled)
No specific diagnostic tests are required, though imaging
(e.g., X-rays, CT scans) is used to assess the underlying fracture. The
blisters are generally painless, similar to friction blisters or second-degree
burns, but their presence can be daunting for patients and inexperienced
clinicians.
Managing Fracture Blisters
The management of fracture blisters is a complex and
controversial topic, with no universal consensus in the medical literature. The
primary challenge is balancing the need for timely fracture stabilization with
the protection of compromised skin to minimize complications.
General Principles
- Intact
Blisters:
- Should
be left undisturbed, as the blister roof serves as a sterile biological
dressing, reducing infection risk (Healthline).
- Gentle,
non-adherent dressings (e.g., Aquacel, gauze) can be applied to protect
the area.
- Ruptured
Blisters:
- Require
cleaning and dressing with moist, non-occlusive dressings to promote
healing.
- Topical
agents like silver sulfadiazine (Silvadene) are commonly used to prevent
infection and aid re-epithelialization, particularly in non-diabetic
patients (PubMed Study).
- Silver-coated
dressings may reduce pain and shorten healing time.
Surgical Considerations
- Delaying
Surgery:
- Most
experts recommend delaying surgical fixation until blisters resolve,
typically 7–10 days, to reduce the risk of wound complications (PMC Article).
- Average
delays vary by fracture type:
|
Fracture Type |
Average Delay (Days) |
|
Ankle | 6 |
|
Tibial Plateau |
11 |
|
Tibial Shaft |
3.5 |
|
Calcaneal |
12 |
|
Pilon |
6.75 |
|
Mean |
7.7 |
- Early
Surgery:
- In
high-energy trauma, surgery within 24–48 hours may stabilize the fracture
and reduce further soft-tissue damage, potentially preventing blister
formation.
- Incisions
should avoid blister beds, as crossing them can double the risk of
infection and wound dehiscence.
- Alternative
Approaches:
- If
surgery is urgent, incisions can be made through the blister bed (less
preferred) or planned to avoid blisters entirely.
- The
AO Foundation recommends waiting 7–10 days for non-urgent surgeries if
blisters are present.
Advanced Techniques
- Negative
Pressure Wound Therapy (NPWT):
- Also
known as a “wound vac,” NPWT may accelerate blister healing, allowing
earlier surgical intervention (Verywell Health).
- Blister
Aspiration or Deroofing:
- Some
studies support aspirating or deroofing blisters and treating the bed
with antimicrobials, but this should be done cautiously due to infection
risks (EFORT Open Reviews).
- A
2025 systematic review found evidence supporting this approach in
controlled settings.
Patient-Specific Factors
Patients with comorbidities like diabetes or vascular
disease require close monitoring and may need hospital admission if blisters
develop. Early recognition and tailored wound care are critical in these
high-risk groups.
Potential Complications
Fracture blisters can significantly complicate fracture
management:
- Infection:
Ruptured blisters or incisions through blister beds increase the risk of
bacterial colonization and surgical site infections.
- Wound
Dehiscence: Surgical wounds may fail to heal properly, leading to
prolonged recovery.
- Delayed
Healing: Both the fracture and skin may take longer to heal, extending
hospital stays.
- Chronic
Ulcers: Rare but possible in severe cases.
- Scarring
and Pigmentation Changes: More common with blood-filled blisters due
to deeper tissue damage.
A study by Strauss et al. reported a 13% prevalence of wound
complications in 45 patients with lower extremity fracture blisters.
Blood-filled blisters are particularly concerning, with six out of seven skin
complications in one study requiring split-thickness skin grafting.
Preventing Fracture Blisters
While not always preventable, early surgical stabilization
within 24 hours of injury may reduce blister formation by minimizing ongoing
soft-tissue trauma. This is particularly relevant for high-energy injuries.
Additionally, careful monitoring of high-risk patients and prompt wound care
can mitigate complications.
Fracture blisters are a fascinating yet challenging aspect
of orthopedic trauma. They highlight the intricate relationship between bone
and soft tissue in the healing process. For patients, understanding fracture
blisters can demystify a potentially alarming complication, while for
healthcare providers, it underscores the need for careful, individualized
management. By respecting the blisters’ role as a natural barrier, avoiding
unnecessary interventions, and prioritizing wound care, we can optimize outcomes
for patients with fractures.
Whether you’re a patient navigating recovery or a clinician
managing complex cases, fracture blisters remind us that even the smallest
details—like a blister on the skin—can have a big impact on healing.

Comments
Post a Comment