Tuberculosis: Understanding its Testing Methods and Treatments - By Dr Markandaiya Acharya
Tuberculosis (TB) is a contagious bacterial infection that predominantly affects the lungs but can potentially affect other organs. The bacteria Mycobacterium tuberculosis causes it, and it spreads through the air when an infected person coughs, sneezes, or talks. In this post, we will look at the various tuberculosis therapies available, as well as the skin and Montaux tests used for diagnosis and the TB vaccination for prophylaxis.
Introduction
Tuberculosis (TB) is a contagious bacterial infection that predominantly affects the lungs but can potentially affect other organs. The bacteria Mycobacterium tuberculosis causes it, and it spreads through the air when an infected person coughs, sneezes, or talks. In this post, we will look at the various tuberculosis therapies available, as well as the skin and Montaux tests used for diagnosis and the TB vaccination for prophylaxis.
(Tuberculosis public health campaign in Ireland, 1905)
Understanding Tuberculosis
What is Tuberculosis?
Tuberculosis (TB) is an infectious disease caused by the bacteria Mycobacterium tuberculosis. It primarily affects the lungs, although it can also damage the kidneys, spine, and brain. TB spreads through the air when an infected person exhales respiratory droplets that others around can inhale.
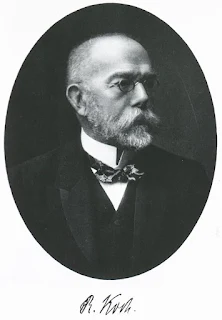
(Robert Koch discovered the tuberculosis bacillus.)
Causes and Transmission
Mycobacterium tuberculosis is the microorganism that causes tuberculosis. The bacteria are released into the air when an infected person coughs, sneezes, or speaks. People in close proximity to the bacteria may breath them and become ill. It is vital to highlight that tuberculosis is not easily spread and usually necessitates lengthy and close contact with an infected person.
Symptoms and Diagnosis
Tuberculosis symptoms include
- prolonged coughing,
- chest pain,
- weight loss,
- exhaustion,
- fever, and
- night sweats.
TB can be diagnosed using a variety of techniques, including
(An anteroposterior X-ray of a patient diagnosed with advanced bilateral pulmonary tuberculosis. This AP X-ray of the chest reveals the presence of bilateral pulmonary infiltrate (white triangles), and „caving formation“ (black arrows) present in the right apical region. The diagnosis is far-advanced tuberculosis.)
- imaging investigations (like XRAYS & MRI),
- sputum testing, and
- tuberculin skin tests.
Treatments for Tuberculosis
Tuberculosis can be treated using a mix of antibiotics to guarantee that the germs are eradicated completely.
The treatment is usually divided into two stages:
- the initial phase and
- the continuation phase.
If the infection is drug-resistant, second-line medications may be required in some circumstances.
Skin Test for Tuberculosis
What is the Skin Test?
How do we perform Tuberculin skin test?
1. An induration of 5 or more millimeters is considered positive in the following groups:
2. An induration of 10 or more millimeters is considered positive in the following groups:
3. An induration of 15 or more millimeters is considered positive in people with no known risk factors for TB.
Tuberculosis Vaccine (BCG Vaccine)
Understanding the BCG Vaccine
The Bacillus Calmette-Guérin (BCG) vaccine is a tuberculosis vaccine. It is made from a weakened strain of Mycobacterium bovis, which is linked to Mycobacterium tuberculosis. The BCG vaccine boosts the immune system to guard against tuberculosis.
Vaccination Process
In tuberculosis-endemic nations, the BCG vaccine is frequently provided during childhood. The vaccination is injected just beneath the skin in a little dose. The immune system develops a response that helps defend against tuberculosis infection over time.
(An apparatus (4–5 cm length, with 9 short needles) used for BCG vaccination in Japan, shown with ampules of BCG and saline)
Efficacy and Limitations
While the BCG vaccine provides some protection against severe tuberculosis in children, its efficacy against adult pulmonary tuberculosis is varied. The vaccination is more successful in avoiding severe types of tuberculosis in children, such as meningitis and disseminated illness.
Conclusion
Tuberculosis is a dangerous infectious disease that must be diagnosed and treated as soon as possible. Understanding the various treatment options, such as first-line and second-line medications, is critical for effective management. Furthermore, the Montaux and skin tests provide crucial diagnostic information, assisting in early detection and intervention. Furthermore, the BCG vaccine is critical in avoiding serious tuberculosis, particularly in high-risk areas. We can work towards a world free of tuberculosis by raising awareness, improving access to healthcare, and implementing preventive measures.
Frequently Asked Questions (FAQs)
1. Q: Is tuberculosis a highly contagious disease?
2. Q: Can tuberculosis be completely cured?
A: With proper treatment and adherence to medication, tuberculosis can be cured in the majority of cases.
3. Q: Are there any side effects of the BCG vaccine?
A: Common side effects of the BCG vaccine include a localized skin reaction at the injection site and swollen lymph nodes.
4. Q: Can tuberculosis be transmitted through sharing food or drinks?
A: No, tuberculosis is primarily transmitted through respiratory droplets and does not spread through sharing food or drinks.
5. Q: Is tuberculosis more common in certain regions of the world?
A: Tuberculosis is more prevalent in areas with limited access to healthcare, overcrowding, and poor sanitation.







Comments
Post a Comment