Kidney Stones: Causes, Treatments, Prevention Strategies, and Long-Term Outcomes
Kidney stones, medically known as nephrolithiasis or urolithiasis, are hard deposits of minerals and salts that form in the kidneys. Affecting approximately 1 in 11 people in the United States, kidney stones represent a significant public health challenge, with the prevalence increasing globally due to factors such as dietary habits and lifestyle changes. These stones can range in size from tiny crystals to large, pebble-like formations that can cause excruciating pain, urinary complications, and even long-term kidney damage if left untreated.
Image: A 39 year old man presents to the Emergency Department with a 5 hour history of right sided abdominal pain. He describes it as "coming in waves" and being the most severe pain he has ever experienced.
Understanding the formation, treatment options, and
prevention strategies for kidney stones is crucial not only for those currently
affected but also for people at risk. Effective management can prevent serious
complications, such as chronic kidney disease (CKD) or end-stage renal disease
(ESRD). As kidney stones often recur, developing a comprehensive approach to
prevention is vital for improving quality of life and reducing healthcare
costs.
Causes and Risk Factors
Kidney stones are caused by a complex interplay of factors,
including metabolic, lifestyle, and genetic elements. To better understand
these triggers, we must first look at how these factors work together to
promote stone formation.
Image: Showing Multiple Renal stones
Metabolic Disorders and Kidney Stone Formation
Certain metabolic disorders significantly raise the risk of
kidney stones. Conditions such as hypercalciuria (excess calcium in the
urine), hyperoxaluria (excess oxalate), and hypocitraturia (low
citrate levels) create an environment conducive to stone formation. Calcium
stones, the most common type, form when the concentration of calcium in the
urine exceeds the body's ability to dissolve it.
For instance, hyperoxaluria often results from a diet
rich in oxalates, such as spinach, nuts, and tea, which can contribute to the
formation of calcium oxalate stones. Likewise, hypercalciuria, which can
be hereditary, leads to an increased risk of stone recurrence. Metabolic
conditions like gout also increase uric acid levels, which can
crystallize into stones.
Lifestyle Factors
Lifestyle choices play a substantial role in kidney stone
formation. Dehydration is a leading contributor; insufficient fluid
intake concentrates the urine, which encourages mineral crystallization. A high-sodium
diet promotes calcium excretion in the urine, increasing the risk of
calcium stones. Similarly, excessive consumption of animal protein
raises the levels of calcium, oxalate, and uric acid, all of which contribute
to stone formation.
Obesity has also been linked to an increased likelihood of
kidney stones. Studies show that obese individuals are more likely to develop
stones due to metabolic changes that affect how the body processes calcium and
other minerals. Maintaining a healthy weight can reduce the risk of stone
development.
Genetic Predisposition and Family History
Family history plays a crucial role in determining the risk
of kidney stones. Genetic predisposition can influence several aspects
of stone formation, including urine composition and metabolic factors.
Individuals with a family history of kidney stones are at a higher risk,
suggesting that hereditary factors may affect how the body handles calcium and
oxalate.
Symptoms and Signs of Kidney Stones
Kidney stones may remain asymptomatic until they start to
move within the kidney or pass into the ureters (the tubes connecting the
kidneys to the bladder). Once a stone starts moving, it can cause a range of
symptoms.
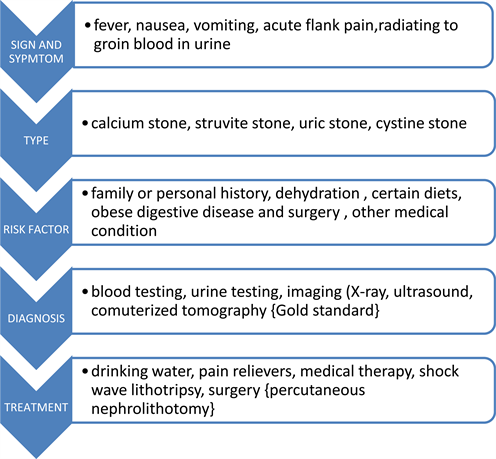
Image: Symptoms of Renal stones
1. Severe Pain (Renal Colic)
The hallmark symptom of kidney stones is severe pain,
often referred to as renal colic. The pain can be sudden and sharp,
varying in intensity and location, depending on where the stone is located in
the urinary tract.
- Location
of Pain: The pain typically begins in the flank (the area
between the ribs and hip), often radiating to the lower abdomen and groin
as the stone moves down the ureter. This pain pattern follows the path of
the urinary tract and can shift as the stone moves through the system.
- Characteristics
of Pain: Patients describe the pain as severe, unrelenting, and
spasmodic. It can come in waves (lasting 20 to 60 minutes), as the body
tries to push the stone down the urinary tract. The pain can also worsen
or subside as the stone shifts positions within the ureter.
2. Hematuria (Blood in the Urine)
Hematuria is another common symptom of kidney stones,
occurring when the stone irritates the lining of the urinary tract. Blood in
the urine can range from being microscopic (visible only under a
microscope) to gross hematuria (where the blood is visible to the naked
eye, causing the urine to appear pink, red, or brown).
- Microscopic
Hematuria: This is often detected during urinalysis and may be the
first sign of kidney stones, especially in asymptomatic patients.
- Gross
Hematuria: In more severe cases, the presence of blood in the urine
may be obvious and may occur with or without pain.
3. Nausea and Vomiting
Severe kidney pain can stimulate the nerves in the
gastrointestinal tract, leading to nausea and vomiting. This is
especially common during episodes of intense renal colic, as the body’s
autonomic response to the extreme pain causes discomfort in other organs.
4. Urinary Symptoms
When a stone is lodged in the lower ureter, near the
bladder, patients may experience a variety of urinary symptoms:
- Frequent
Urination: The stone’s irritation to the bladder wall can create a
sensation of needing to urinate frequently, even if the bladder is not
full.
- Urgency:
Patients may feel an urgent need to urinate but pass only small amounts of
urine.
- Dysuria
(Painful Urination): Stones near the bladder can cause burning or
discomfort during urination.
5. Cloudy or Foul-Smelling Urine
In some cases, kidney stones can lead to urinary tract
infections (UTIs), which present with symptoms such as cloudy or
foul-smelling urine. If an infection accompanies a kidney stone, additional
symptoms like fever and chills may also occur, requiring
immediate medical attention.
6. Fever and Chills (Indicative of Infection)
While fever is not a direct symptom of kidney stones, its
presence suggests a concurrent infection, which can be life-threatening if
untreated. A fever, especially when accompanied by chills, could
indicate a kidney infection (pyelonephritis) or sepsis, requiring
urgent medical intervention.
Key Signs to Watch For:
- Severe,
radiating pain that moves from the flank to the lower abdomen or
groin.
- Blood
in the urine, either visible or microscopic.
- Nausea
and vomiting triggered by severe pain.
- Urinary
symptoms like frequency, urgency, or painful urination.
- Fever
and chills, indicating possible infection.
Diagnostic Tests and Investigations
Once a patient presents with the symptoms of kidney stones,
a series of diagnostic tests are performed to confirm the diagnosis, assess the
size and location of the stone, and evaluate any potential complications, such
as obstruction or infection.
Image: Flowchart outlining the progression from symptoms to treatment in a patient with renal colic.
1. Urinalysis
Urinalysis is one of the first diagnostic tests
ordered when kidney stones are suspected. It helps detect abnormalities in the
urine that could indicate the presence of stones, infection, or other urinary
issues.
- Microscopic
Hematuria: Even if the patient does not visibly see blood in their
urine, urinalysis can detect microscopic amounts of blood, which is common
in kidney stone cases.
- Crystalluria:
The presence of crystals (such as calcium oxalate, uric acid, or struvite)
in the urine can help identify the type of stone forming in the kidneys.
- Signs
of Infection: If an infection is present, urinalysis may reveal leukocytes
(white blood cells) and nitrites in the urine, suggesting a
bacterial infection.
2. Blood Tests
Blood tests provide valuable information about the metabolic
abnormalities contributing to stone formation and the patient’s kidney
function.
- Serum
Calcium and Uric Acid Levels: Elevated levels of calcium or uric acid
in the blood can indicate a predisposition to calcium oxalate or uric
acid stones.
- Kidney
Function Tests: Blood tests measuring creatinine and blood
urea nitrogen (BUN) levels help assess overall kidney function. If
kidney function is impaired due to obstruction by a stone, these values
may be abnormal.
3. Imaging Studies
Imaging is the cornerstone of kidney stone diagnosis,
allowing for the visualization of the stone, its size, and its location in the
urinary tract. The most common imaging modalities include:
Non-Contrast Helical CT Scan (CT KUB)
A non-contrast helical computed tomography (CT) scan
of the kidneys, ureters, and bladder (CT KUB) is the gold standard for
diagnosing kidney stones. This type of CT scan does not require the use of
contrast dye, making it safe for patients with allergies or kidney dysfunction.
CT scans can detect stones as small as 1-2 mm and provide information on:
- Stone
Size and Location: A CT scan accurately identifies the exact location
of the stone, whether it is in the kidney, ureter, or bladder.
- Stone
Composition: While CT scans cannot directly identify the stone's
composition, the stone's appearance and location provide clues. For
instance, uric acid stones may appear radiolucent, whereas calcium stones
are more radio-opaque.
Ultrasound
Ultrasound is often used in patients for whom CT
scans are not ideal, such as pregnant women or children. While less sensitive
than a CT scan, ultrasound can detect larger stones in the kidneys and ureters
and is useful for identifying hydronephrosis (swelling of the kidney due
to urine buildup), which indicates obstruction.
- Advantages:
Ultrasound is non-invasive, radiation-free, and widely available.
- Limitations:
It is less accurate for detecting smaller stones, particularly those
located in the ureters.
X-Ray (KUB) and Intravenous Pyelogram (IVP)
A Kidneys-Ureters-Bladder (KUB) X-ray can detect
large stones made of calcium, but it may miss smaller or radiolucent stones
(like uric acid stones). For more detailed imaging, an Intravenous Pyelogram
(IVP), an older imaging technique where a contrast dye is injected into a
vein, allows visualization of the urinary tract on X-ray. However, IVP is
largely being replaced by CT scans due to its superior diagnostic accuracy.
4. Stone Analysis
After a stone has passed or been surgically removed, stone
analysis is performed to determine its composition. Knowing the type of
stone helps guide preventive treatment and dietary modifications to reduce the
risk of recurrence.
- Calcium
Oxalate Stones: The most common type, accounting for approximately 80%
of kidney stones.
- Uric
Acid Stones: Associated with high uric acid levels and acidic urine.
- Struvite
Stones: Often linked to chronic urinary tract infections.
- Cystine
Stones: Rare, caused by a genetic disorder called cystinuria.
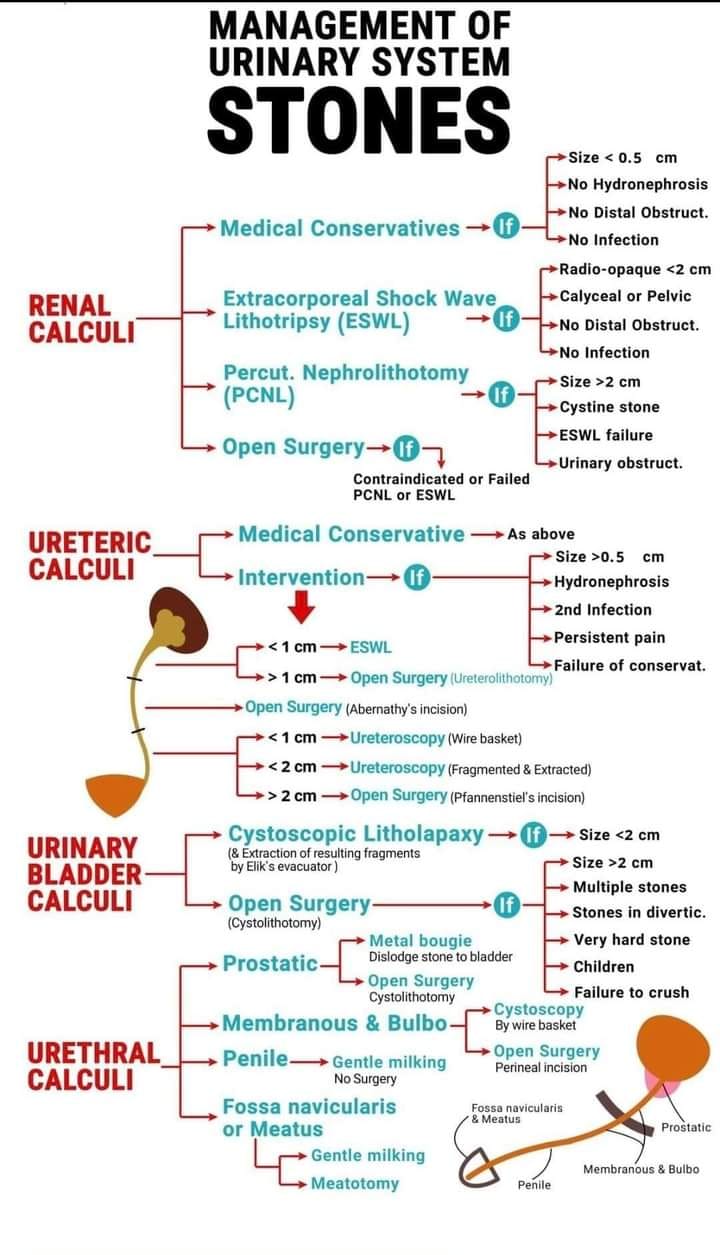
Treatment Options
Treatment options for kidney stones depend on the size,
location, and composition of the stone, as well as the severity of symptoms.
Here, we'll explore both non-invasive and invasive treatments, as well as
emerging technologies.
Medical Management
Pharmacotherapy
For patients with small stones or those at risk of recurrent
stones, medications can play a critical role. Potassium citrate is often
prescribed to alkalize the urine, reducing the likelihood of uric acid and
cystine stone formation. It is particularly effective in cases of hypocitraturia,
a condition characterized by low citrate levels in the urine.
Another medication, thiazide diuretics, helps reduce
calcium levels in the urine, preventing calcium stone formation. Thiazides are
commonly used in patients with hypercalciuria and have been shown to
reduce recurrence rates by nearly 50% in some cases.
Dietary Changes
Diet plays a central role in both preventing and managing
kidney stones. Increasing fluid intake is the most effective strategy to
prevent new stone formation by diluting the substances in urine that lead to
stone formation. Patients are often advised to drink at least 2-3 liters of
water per day to maintain proper hydration levels.
Reducing the intake of oxalate-rich foods, such as
spinach, beets, and nuts, can help prevent the formation of calcium oxalate
stones. Likewise, limiting sodium intake can reduce calcium excretion,
minimizing the risk of stone development.
Surgical Interventions
When stones are too large to pass on their own or cause
severe symptoms, surgical intervention may be necessary. The two most common
procedures are lithotripsy and ureteroscopy.
Lithotripsy
Extracorporeal shock wave lithotripsy (ESWL) is a
non-invasive procedure that uses shock waves to break kidney stones into
smaller fragments, which can then be passed through the urine. ESWL is commonly
used for stones that are less than 2 cm in size and is one of the least
invasive treatments available.
Ureteroscopy
For larger or more complex stones, ureteroscopy may
be required. In this procedure, a thin scope is passed through the urethra into
the bladder and ureter to locate the stone. Once the stone is identified, it
can be either retrieved or broken into smaller pieces using a laser.
Emerging Therapies and Technologies
Recent advancements in laser technologies and minimally
invasive surgeries have improved the outcomes for patients with larger or more
complex stones. Holmium laser lithotripsy, for example, has emerged as a
highly effective method for fragmenting stones with fewer complications.
Image: Kidney stone management
Prevention Strategies
Preventing kidney stones requires a multi-faceted approach
involving dietary changes, medications, and lifestyle modifications. While some
patients may be genetically predisposed to stones, others can reduce their risk
significantly through proper management.
Dietary Modifications
Increased Fluid Intake
The most critical component of kidney stone prevention is
adequate hydration. Drinking sufficient water helps dilute the substances in
urine that lead to stone formation. Aim for at least 2-3 liters of fluid per
day, with higher intake levels during hot weather or strenuous activity.
Reducing Oxalate and Sodium
Reducing oxalate intake is particularly important for those
prone to calcium oxalate stones. Foods high in oxalate, such as spinach,
chocolate, and nuts, should be limited. Additionally, a low-sodium diet can
help reduce calcium excretion in the urine, which lowers the risk of stone
formation.
Pharmacological Interventions
Potassium Citrate
As mentioned earlier, potassium citrate is used to maintain
an alkaline urine pH, which helps prevent uric acid stones. It is especially
useful for patients with hypocitraturia and has been shown to reduce the
recurrence of stones by stabilizing urine chemistry.
Thiazides
Thiazides, commonly used to treat hypertension, are
also effective in reducing calcium levels in the urine. By lowering urine
calcium levels, thiazides help reduce the risk of calcium stone formation,
particularly in patients with hypercalciuria.
Lifestyle Changes
Weight Management
Maintaining a healthy weight can help reduce the risk of
kidney stones. Obesity is linked to metabolic changes that increase the
likelihood of stone formation, making weight management a key prevention
strategy.
Stress Reduction
While not directly linked to stone formation, chronic
stress can exacerbate kidney issues by affecting overall health and
hydration habits. Stress management techniques, such as mindfulness, regular
exercise, and proper sleep, can support kidney health.
Image: Prevention strategies
Long-Term Outcomes and Complications
Kidney stones, if not properly managed, can lead to severe
long-term consequences, including chronic kidney disease (CKD) and end-stage
renal disease (ESRD).
Chronic Kidney Disease (CKD) and Kidney Function Decline
Recurrent kidney stones can damage the kidney tissues,
leading to a gradual decline in kidney function. Studies show that people with
frequent stone episodes have a higher risk of developing CKD, a
condition where the kidneys lose their ability to filter waste from the blood
efficiently.
End-Stage Renal Disease (ESRD) and Transplantation
In extreme cases, patients with recurrent or large stones
may experience kidney failure, requiring dialysis or kidney transplantation.
ESRD is the final stage of CKD and can result from years of untreated or poorly
managed kidney stones.
Quality of Life Implications
Beyond the physical symptoms, kidney stones can have a
profound impact on mental health. Recurrent pain, the need for frequent
medical interventions, and the anxiety of potential complications can
contribute to emotional stress, depression, and a lower quality of life.
Psychological support and counseling can be crucial for patients dealing with
these challenges.
Conclusion
Kidney stones are a complex medical issue that requires
careful management to prevent recurrence and long-term complications.
Understanding the causes, risk factors, and available treatments is essential
for both patients and healthcare providers. Preventive measures, such as
dietary changes, hydration, and medication, can significantly reduce the risk
of stone formation and protect kidney health.
For those who experience recurrent stones, it's vital to
work closely with healthcare providers to monitor kidney function and take
proactive steps to prevent further damage. By prioritizing kidney health,
individuals can avoid the debilitating effects of kidney stones and enjoy a
higher quality of life.
Let this be a call to action for anyone affected by or at
risk of kidney stones: stay hydrated, maintain a healthy diet, and seek
medical advice at the first sign of trouble. Early intervention can make
all the difference in preserving kidney function and long-term health.





Its a very useful article. Very very thanks Sir
ReplyDelete