Pancreatic Cancer: Early Signs, Risks, and Treatment Options
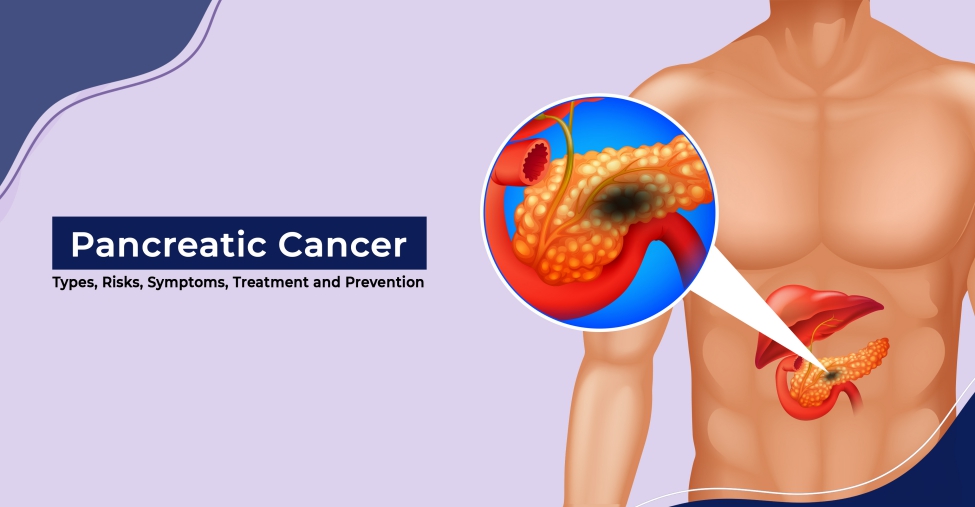
Pancreatic cancer is a life-threatening disease that originates in the tissues of the pancreas, an organ located deep within the abdomen, nestled between the stomach and spine. The pancreas plays a crucial role in the body, producing enzymes that aid digestion and hormones like insulin that regulate blood sugar levels. Pancreatic cancer occurs when the cells in the pancreas undergo genetic mutations, leading them to grow uncontrollably and form a tumor. This type of cancer is particularly dangerous because it often goes undetected until it has reached an advanced stage, making it difficult to treat.
Types of Pancreatic Cancer
Pancreatic cancer is broadly categorized into two types: exocrine tumors and neuroendocrine tumors.
Exocrine tumors: These are the most common, accounting for over 90% of pancreatic cancers. The majority of these are adenocarcinomas, which originate in the ducts of the pancreas that carry digestive enzymes.
Neuroendocrine tumors (NETs): These are much rarer, representing less than 10% of pancreatic cancers. NETs develop from the hormone-producing cells in the pancreas and have a different prognosis and treatment approach compared to exocrine tumors.
Symptoms and Causes
Symptoms
Pancreatic cancer is notorious for being a "silent" disease in its early stages. Most people do not exhibit any symptoms until the cancer has grown large enough to affect surrounding organs. When symptoms do appear, they can be vague and easily attributed to other conditions. Common symptoms include:
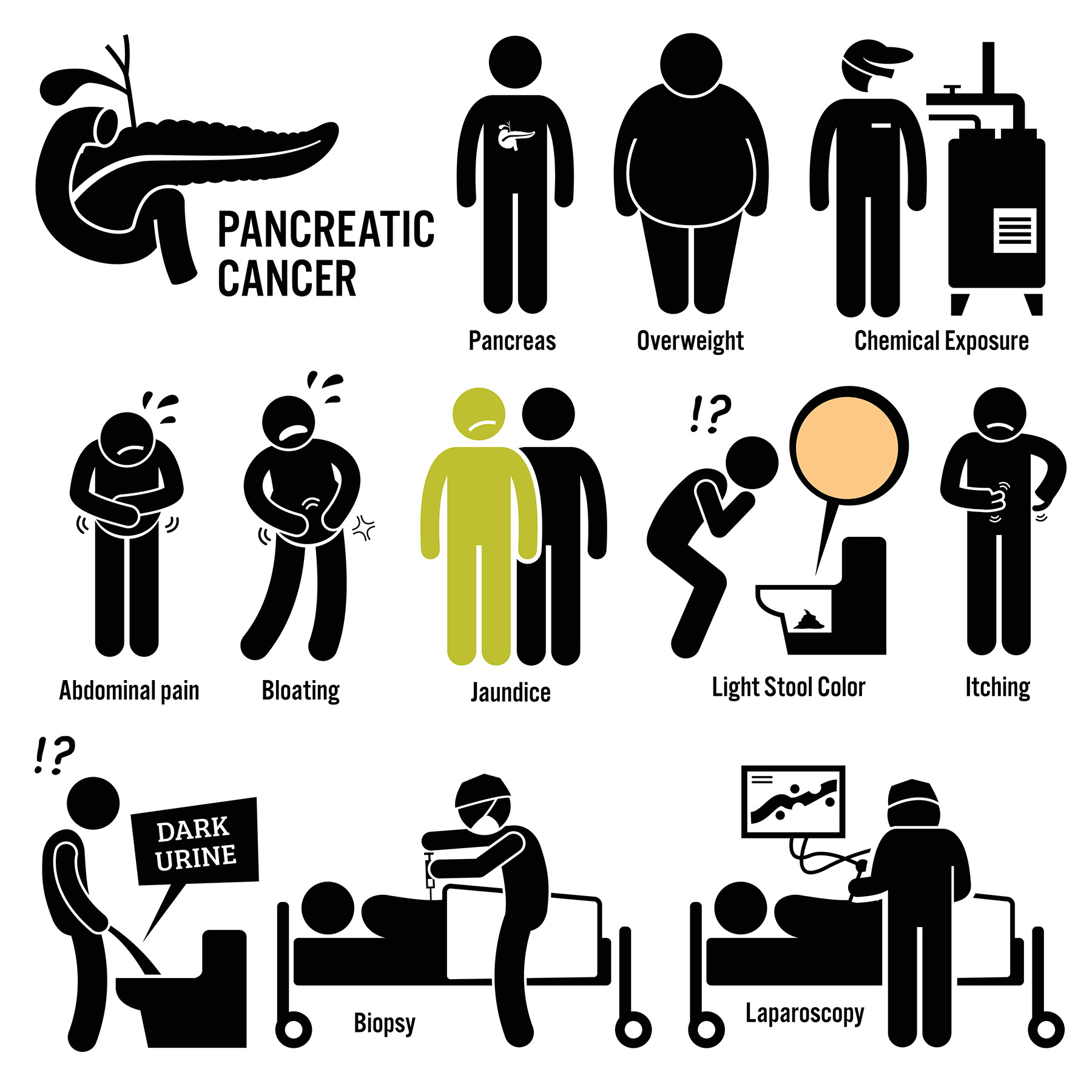
(Symptoms of Pancreatic Cancer)
- Jaundice: A yellowing of the skin and eyes caused by the buildup of bilirubin, a substance produced by the liver.
- Abdominal and back pain: Pain in the upper abdomen that radiates to the back is a common symptom.
- Unexplained weight loss: Rapid and unexplained weight loss is a red flag.
- Digestive issues: Nausea, vomiting, diarrhea, and changes in stool color or consistency.
- Diabetes: New-onset diabetes or worsening control in someone who already has diabetes can be a sign of pancreatic cancer.
- Fatigue: Persistent tiredness and lack of energy.
- Blood clots: Pancreatic cancer can cause blood to clot more easily.
Causes and Risk Factors
The exact cause of pancreatic cancer is still unknown, but certain risk factors have been identified that increase the likelihood of developing this disease. These include:
- Smoking: Tobacco use is one of the most significant risk factors for pancreatic cancer.
- Age: The risk increases with age, particularly after 60.
- Family history: A family history of pancreatic cancer or certain genetic syndromes, such as those involving the BRCA1 or BRCA2 genes, can elevate the risk.
- Chronic pancreatitis: Long-term inflammation of the pancreas has been linked to an increased risk of pancreatic cancer.
- Diabetes: Especially in individuals who develop diabetes later in life without any other underlying cause.
- Obesity: Excess body weight, particularly around the abdomen, is associated with a higher risk.
Diagnosis and Tests
How is Pancreatic Cancer Diagnosed?
Diagnosing pancreatic cancer can be challenging because the pancreas is located deep within the body, and early tumors often do not cause symptoms. When pancreatic cancer is suspected, healthcare providers use a combination of tests to confirm the diagnosis:
- Imaging tests: These include CT scans, MRI, PET scans, and endoscopic ultrasounds, which provide detailed images of the pancreas and surrounding organs.
- Blood tests: Tests such as the CA 19-9 tumor marker can indicate the presence of pancreatic cancer, though they are not definitive on their own.
- Biopsy: A definitive diagnosis usually requires a biopsy, where a small sample of tissue is taken from the pancreas and examined under a microscope.
- Staging laparoscopy: A surgical procedure where a camera is inserted into the abdomen to assess the extent of the cancer.
Genetic Testing
For some patients, genetic testing may be recommended to determine if their pancreatic cancer is linked to inherited genetic mutations. This information can be crucial for guiding treatment decisions and understanding the risk for family members.
Management and Treatment
Is Pancreatic Cancer Curable?
Pancreatic cancer is often difficult to cure, primarily because it is usually diagnosed at a late stage. However, if caught early, there is a possibility of complete remission, especially if the cancer can be surgically removed.
Treatment Options
The treatment plan for pancreatic cancer depends on several factors, including the stage of the cancer, the location of the tumor, and the overall health of the patient. Common treatment options include:
- Surgery: Surgery offers the best chance for a cure but is only an option if the cancer has not spread extensively. The Whipple procedure is the most common surgery, involving the removal of the head of the pancreas, part of the bile duct, the gallbladder, and portions of the stomach and small intestine.
- Chemotherapy: Often used in conjunction with surgery, chemotherapy involves using drugs to kill cancer cells or slow their growth.
- Radiation therapy: This treatment uses high-energy beams to target and destroy cancer cells. It is sometimes combined with chemotherapy.
- Targeted therapy: These treatments target specific abnormalities within cancer cells. Drugs like erlotinib, olaparib, and others are used depending on the genetic profile of the tumor.
- Pain management: Managing pain is a critical aspect of treatment, especially for advanced pancreatic cancer. Pain relief can be achieved through medications, nerve blocks, or other interventions.
Prevention
Can Pancreatic Cancer Be Prevented?
(Prevention of Pancreatic Cancer)
There is no guaranteed way to prevent pancreatic cancer, but several lifestyle changes can reduce the risk:
- Quit smoking: Smoking is the most significant modifiable risk factor.
- Healthy diet: Eating a diet rich in fruits, vegetables, and whole grains while reducing red meat and processed foods can lower the risk.
- Maintain a healthy weight: Obesity is a known risk factor, so maintaining a healthy weight is important.
- Regular exercise: Physical activity can help reduce the risk of pancreatic cancer and many other diseases.
- Limit alcohol consumption: Excessive drinking can lead to chronic pancreatitis, which increases the risk of pancreatic cancer.
ALSO READ: Triumph Over Adversity: The Story of Phocomelia and the Remarkable Journey of India’s Sheetal Devi
Screening and Early Detection
Routine screening for pancreatic cancer is not typically recommended for the general population. However, individuals with a high risk, such as those with a family history or genetic predispositions, may benefit from regular monitoring through imaging tests or endoscopic ultrasounds.
Outlook / Prognosis
What Can You Expect?
A diagnosis of pancreatic cancer can be overwhelming, but understanding the disease and its progression can help patients and their families prepare for what lies ahead. The prognosis for pancreatic cancer is generally poor, with a five-year survival rate of around 11%. However, survival rates can vary widely depending on the stage at diagnosis and the patient's response to treatment.
Living with Pancreatic Cancer
Living with pancreatic cancer requires a comprehensive approach to care, including managing symptoms, undergoing treatment, and seeking emotional and psychological support. Patients are encouraged to maintain open communication with their healthcare team, participate in support groups, and seek counseling if needed.
ALSO READ: 1 in 3 patients develop antidepressant withdrawal syndrome
Conclusion
Pancreatic cancer is a challenging and often aggressive disease, but advances in research and treatment are offering new hope. Early detection, although difficult, is key to improving outcomes. By understanding the risk factors, recognizing symptoms, and exploring all available treatment options, patients can take an active role in managing their health and improving their quality of life.


Comments
Post a Comment