Sinusitis Demystified: It's Symptoms, Causes, and Effective Treatments
Sinusitis, also known as a sinus infection, occurs when the tissue lining the sinuses becomes inflamed or swollen, leading to congestion, discomfort, and other symptoms. The sinuses are air-filled cavities located behind the forehead, cheeks, and eyes, and they produce mucus that helps keep the nasal passages clean. When these passages become blocked due to infection or allergies, it can lead to sinusitis.
Sinusitis is one of the most common health conditions,
affecting approximately 30 million adults in the U.S. each year. The
condition ranges from a mild annoyance to a severe, debilitating illness,
impacting both personal and professional life. Chronic sinusitis, in
particular, can persist for weeks or even months, leading to recurrent
infections, headaches, and impaired quality of life.
Symptoms of Sinusitis
Common Symptoms
Sinusitis often presents with symptoms that overlap with
other respiratory conditions, making it tricky to diagnose without medical
evaluation. Common signs include:
Image: Showing the symptoms of Sinusitis
- Nasal
congestion: Blocked nasal passages that make breathing difficult.
- Sinus
pressure: A feeling of heaviness or pain around the eyes, forehead,
and cheeks.
- Headaches:
Often worse in the morning, increasing when bending over.
- Postnasal
drip: Mucus dripping down the back of the throat, causing irritation.
- Fatigue:
Due to the body's immune response to infection.
- Fever:
Particularly in cases of bacterial sinusitis.
Chronic Sinusitis Symptoms in Adults
When sinusitis lasts longer than 12 weeks, it is
classified as chronic. Symptoms in adults may include:
- Persistent
nasal blockage.
- Reduced
sense of smell and taste.
- Thick,
discolored mucus.
- Facial
pain and pressure that worsens throughout the day.
Sinusitis Symptoms in Children
Children may exhibit similar symptoms but might not be able
to express them clearly. Additional signs to watch for include:
- Headache
- Difficulty
feeding.
- Irritability.
- Chronic
cough, especially at night.
- Swollen
or puffy eyelids.
Causes of Sinusitis
Allergies
Seasonal allergies, such as hay fever (allergic
rhinitis), can lead to sinusitis by causing swelling in the nasal passages,
which blocks mucus drainage and creates an environment for infection.
Deviated Septum
A deviated septum, which is an abnormality in the
nasal structure, can restrict airflow and lead to chronic sinusitis due to
improper drainage of mucus.
Cold and Flu
Viral infections like the common cold or the flu
often lead to swelling in the sinuses. When mucus builds up and cannot escape,
it increases the risk of secondary bacterial infections.
Environmental Factors
Exposure to pollutants, secondhand smoke, or dry
air can irritate the nasal passages, leading to inflammation and increased
susceptibility to sinus infections.
Image: Showing how does Sinusitis occur
Types of Sinusitis
Acute vs. Chronic Sinusitis
- Acute
sinusitis: Typically lasts less than 4 weeks and is often triggered by
a viral infection like the cold.
- Chronic
sinusitis: Lasts 12 weeks or more and can be caused by long-term
conditions like allergies or structural issues in the nose.
Differences in Symptoms and Treatment
- Acute
sinusitis often resolves on its own or with minimal treatment, such as over-the-counter
decongestants.
- Chronic sinusitis may require a combination of treatments, including prescription medications or even surgical intervention in severe cases.
Investigations and Diagnosis Methods of Sinusitis
Accurately diagnosing sinusitis involves a combination of
clinical evaluation, medical history, and various diagnostic tests. The goal is
to differentiate sinusitis from other conditions with similar symptoms,
identify the underlying cause (whether viral, bacterial, or allergic), and
determine the appropriate treatment. Below is an overview of the primary
investigations and diagnostic methods used to assess sinusitis.
1. Clinical Examination
The first step in diagnosing sinusitis is a thorough physical
examination by a healthcare provider. This typically includes:
- Medical
history: The doctor will ask about symptoms (e.g., nasal congestion,
facial pain, and postnasal drip) and how long they’ve persisted. A key
factor is whether the symptoms have lasted more than 10 days without
improvement, which suggests bacterial sinusitis.
- Physical
inspection: The doctor may check for signs of nasal swelling, redness,
or discharge. They may also press on the face to identify areas of
tenderness over the sinuses, which could indicate inflammation or
infection.
2. Nasal Endoscopy
A more detailed examination of the sinuses can be performed
using a nasal endoscopy. This involves inserting a thin, flexible tube
with a camera (called an endoscope) into the nose to get a clear view of the
sinus passages and detect blockages or abnormalities. It allows the doctor to:
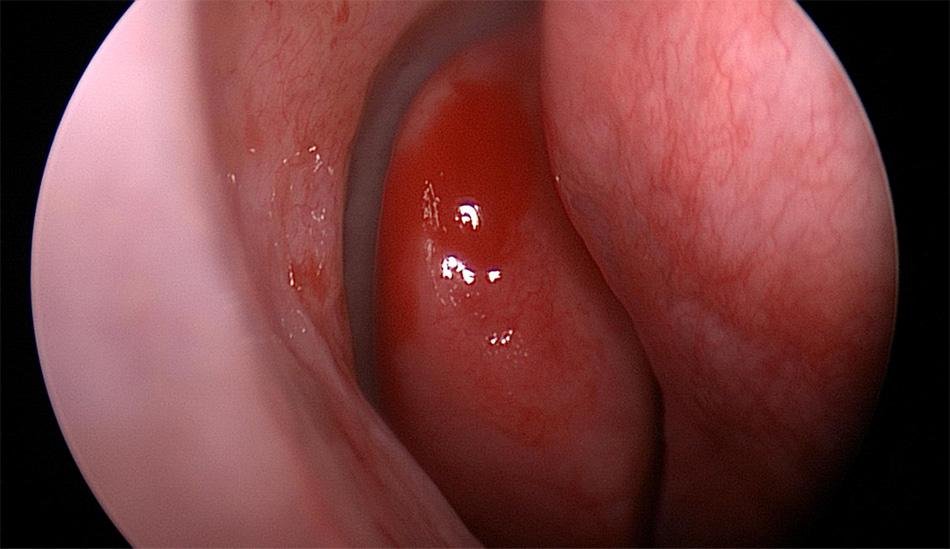
Image: Endoscopic View showing inflamed nasal Mucosa
- Visualize
inflamed sinus tissues.
- Check
for structural issues like a deviated septum or nasal polyps.
- Identify
the presence of pus or thick mucus, indicating infection.
3. Imaging Studies
If the physical exam and nasal endoscopy don't provide
sufficient information, imaging studies may be ordered to get a better
view of the sinuses.
- CT
(Computed Tomography) Scan: A CT scan is the most common imaging
method used to diagnose sinusitis. It provides detailed cross-sectional
images of the sinuses and can reveal:
- Blockages
in the sinus cavities.
- Fluid
buildup or thickened sinus linings.
- Structural
issues such as a deviated septum or nasal polyps.
- The
extent of inflammation and any complications, such as the infection
spreading to surrounding areas.
- MRI
(Magnetic Resonance Imaging): While less commonly used than CT scans,
MRIs may be recommended if there is a suspicion of tumors or fungal sinus
infections, or if a more detailed view of soft tissue structures is
needed.
4. Laboratory Tests
Laboratory tests are generally not needed for routine
sinusitis diagnosis but can be useful in certain cases, particularly when the
cause of sinusitis is unclear or when the condition persists despite treatment.
- Mucus
culture: In cases of chronic or recurrent sinusitis, the doctor may
collect a sample of mucus from the nose for laboratory analysis. This test
can help determine whether the infection is caused by bacteria or fungi,
which guides the choice of antibiotics or antifungal treatment.
- Allergy
testing: If allergies are suspected to be the cause of chronic or
recurring sinusitis, allergy testing (such as skin prick tests or blood
tests) may be conducted to identify specific allergens like pollen,
dust mites, or mold.
5. Sinus Puncture and Aspiration (Rarely Used)
In rare or complicated cases where other diagnostic methods
fail to provide clarity, a sinus puncture and aspiration may be
performed. This involves inserting a needle into the sinus cavity to remove
fluid, which is then tested for bacterial or fungal infections. While highly
accurate, this procedure is invasive and is usually reserved for severe or
treatment-resistant cases of sinusitis.
6. Blood Tests
In severe cases or when complications are suspected, doctors
may order blood tests to check for signs of an immune deficiency, which
can make a person more prone to sinus infections. Blood tests can also check
for markers of inflammation or infection, such as:
- Complete
Blood Count (CBC): To detect elevated white blood cells, which could
indicate an ongoing infection.
- C-reactive
protein (CRP) or Erythrocyte Sedimentation Rate (ESR): These
tests measure inflammation levels in the body and can indicate the
presence of a significant infection.
7. Testing for Chronic Sinusitis
In cases of chronic sinusitis, the diagnostic process
may include additional evaluations to identify underlying causes or
contributing factors such as:
- Immune
system evaluation: Testing to check for immune deficiencies, which
could predispose a person to recurrent sinus infections.
- Gastroesophageal
reflux disease (GERD): Sometimes, GERD or acid reflux can cause or
worsen sinusitis. Investigating GERD might be necessary if sinusitis
persists despite typical treatments.
8. Allergy Testing and Rhinitis Assessment
For patients who suffer from chronic or recurring sinusitis,
allergy testing is often recommended. Since allergic rhinitis
(allergy-related nasal inflammation) is a common trigger for sinus infections,
identifying and managing allergies can be key to preventing sinusitis.
- Skin
prick testing: A small amount of allergen is applied to the skin, and
the reaction is monitored to determine if the patient has an allergic
response.
- Serum-specific
IgE testing: A blood test that detects specific allergy-related
antibodies, useful in cases where skin testing cannot be performed.
Natural Treatment Options
For those seeking natural sinus relief, several home
remedies can help reduce symptoms and improve comfort without the need for
pharmaceuticals.
Home Remedies
- Steam
inhalation: Breathing in steam from a hot shower or a bowl of boiling
water can help to thin mucus and relieve sinus pressure.
- Saline
rinse: Using a saline solution in a neti pot or nasal spray can
flush out mucus and reduce inflammation.
Herbal Supplements
- Turmeric:
Known for its anti-inflammatory properties, turmeric may help alleviate
sinus congestion.
- Ginger:
Often used in teas or supplements, ginger has antimicrobial and
anti-inflammatory benefits that can support sinus health.
Lifestyle Changes
- Diet:
Eating anti-inflammatory foods like leafy greens, berries, and
omega-3-rich fish may help reduce chronic sinus inflammation.
- Exercise:
Regular physical activity promotes circulation and can improve nasal
airflow, alleviating some sinus symptoms.
Medical Treatment Options for Sinusitis
Effective treatment for sinusitis, particularly acute
bacterial rhinosinusitis (ABRS), involves a combination of empiric
antibiotic therapy, symptom management, and adjunctive treatments. The choice
of therapy depends on the severity of symptoms, patient risk factors, and
underlying causes of the infection. Below is a detailed overview of recommended
treatment options, including antibiotics, pain relief medications, and other
supportive therapies.
1. Empiric Antibiotic Therapy
When to Start Antibiotics
Empiric antibiotic therapy should be initiated as soon as
a clinical diagnosis of ABRS is established. ABRS is typically diagnosed
based on symptoms persisting for more than 10 days without improvement, severe
symptoms (such as high fever and facial pain), or worsening symptoms after an
initial improvement following a viral upper respiratory infection.
2. Recommended Antibiotics for ABRS
Amoxicillin-clavulanate is the preferred empiric
antibiotic for treating adults with ABRS. This combination is effective against
a broad range of bacteria that cause sinus infections. The standard dose is:
Image: Showing dosage of Amoxicillin -clavulanate in treatment of sinusitis
- Amoxicillin-clavulanate
(500 mg/125 mg or 875 mg/125 mg): Taken twice daily for 5–7
days in cases of uncomplicated ABRS.
For more severe cases, or in patients with risk factors such
as recent hospitalization, immunocompromised status, or systemic toxicity
(fever >39°C/102°F), a high-dose regimen is recommended:
- High-dose
amoxicillin-clavulanate (2 g orally twice daily) or 90 mg/kg/day
orally twice daily: This is reserved for patients who are at higher
risk for complications or resistance due to factors like:
- Attendance
at daycare.
- Age
younger than 2 years or older than 65 years.
- Recent
antibiotic use within the past month.
3. Treatment for Penicillin-Allergic Patients
For patients allergic to penicillin, alternative antibiotics
are recommended:
- Doxycycline
(100 mg every 12 hours): Effective for ABRS and used as an alternative
to amoxicillin-clavulanate.
- Respiratory
fluoroquinolones:
- Levofloxacin
(500 mg daily) or
- Moxifloxacin
(400 mg daily): These are recommended for patients who cannot
tolerate penicillin-based treatments or in cases where multidrug
resistance is a concern.
4. Treatment Failure
If symptoms persist or worsen after 7 days of antibiotic
treatment, the patient should be reassessed to ensure that ABRS is the correct
diagnosis and to rule out complications.
- Failure
to improve: Defined as no significant reduction in symptoms after 7
days of treatment. This may indicate the need to change the antibiotic
therapy.
- Worsening:
If symptoms progress (e.g., increased fever, facial pain, or new
symptoms), treatment failure is suspected.
In cases of treatment failure, second-line antibiotics
should be used:
- High-dose
amoxicillin-clavulanate: (2 g orally twice daily or 90 mg/kg/day).
- Levofloxacin
(500 mg daily) or moxifloxacin (400 mg daily).
- Clindamycin
(300 mg every 12 hours) combined with a third-generation cephalosporin
like:
- Cefixime
(200 mg every 12 hours) or
- Cefpodoxime
(200 mg every 12 hours).
5. Ancillary (Supportive) Therapies
While antibiotics treat the infection, additional therapies
can provide symptomatic relief and help improve overall recovery.
a.
Decongestants
- Topical
decongestants (e.g., oxymetazoline or xylometazoline):
These are effective in reducing nasal congestion in patients with severe
obstruction. They should be used cautiously and only for short durations
(no more than 5 days) to prevent rebound congestion.
- Use
with caution in patients with hypertension or cardiovascular
disease.
b. Analgesics
For pain relief, nonsteroidal anti-inflammatory drugs
(NSAIDs) are recommended:
- Paracetamol
(500 mg three times a day) or Diclofenac (50 mg three times a day):
Both are effective for managing headaches, facial pain, and discomfort
associated with sinusitis.
c.
Antihistamines
Routine use of antihistamines is not recommended
in patients with ABRS unless there is an underlying allergic component to the
condition, as they may dry out the nasal passages and worsen congestion.
d. Intranasal Corticosteroid Sprays
Although not essential for all cases of ABRS, intranasal
corticosteroid sprays (INCS) are beneficial as an adjunct to antibiotics,
particularly for patients with underlying inflammation or allergic rhinitis.
Common options include:
- Fluticasone
or Mometasone: These sprays are recommended twice daily for 10
days to help reduce inflammation in the nasal passages.
e.
Steam Inhalation
Steam inhalation helps thin mucus and ease sinus congestion.
It is recommended twice a day for 5–7 days to provide relief.
f.
Nasal Saline Irrigation
Saline irrigation using physiologic or hypertonic
saline can assist in clearing mucus and improving nasal airflow. This
treatment is recommended as an adjunctive therapy for patients with ABRS and
can be performed using:
- Nasal
sprays or douching with saline.
Prevention Strategies
Allergy Management
Keeping allergies under control with antihistamines
or allergy shots (immunotherapy) can reduce the likelihood of sinusitis
caused by allergic reactions.
Environmental Control
- Minimize
exposure to pollutants.
- Use
air purifiers to remove allergens like pollen and dust.
- Maintain
proper humidity levels in your living space to prevent dryness that can
irritate the sinuses.
Healthy Habits
- Drink
plenty of water to keep mucus thin.
- Avoid
smoking and secondhand smoke, which can irritate the
sinuses.
- Practice
good hygiene, such as frequent hand washing, to reduce the risk of
catching colds or the flu.
Complications of Untreated Sinusitis
If left untreated, sinusitis can lead to serious health
complications, including:
Infections
Untreated sinusitis can spread to the eyes, brain, or bones,
leading to orbital cellulitis, meningitis, or osteomyelitis.
Abscesses
In rare cases, the infection can form an abscess, requiring
drainage and more aggressive treatment.
Respiratory Issues
Chronic sinusitis can exacerbate conditions like asthma or lead to bronchitis, particularly if postnasal drip irritates the airways.
Special Considerations
Sinusitis During Pregnancy
Pregnant women are more prone to sinus infections due to
hormonal changes that cause nasal swelling. Treatment must be approached
cautiously, with a focus on natural remedies and safe medications like saline
sprays and steam inhalation.
Sinusitis with Deviated Septum
A deviated septum can cause recurrent sinusitis. In severe
cases, septoplasty (surgical correction) may be necessary to improve
airflow and reduce the frequency of infections.
Sinusitis and Allergies
Managing allergies is crucial in preventing sinusitis.
Long-term use of nasal corticosteroids or antihistamines can be
helpful in reducing allergic reactions and preventing subsequent sinus
infections.
Conclusion
Sinusitis can range from a minor inconvenience to a serious,
chronic condition affecting your quality of life. Recognizing the symptoms,
understanding the causes, and knowing both natural and medical treatment
options are key to managing sinusitis effectively. Whether you’re looking for natural
sinus relief or need medical advice, this guide provides comprehensive
insight into every aspect of sinusitis.
For those suffering from persistent or severe sinus
symptoms, it’s essential to consult with a healthcare provider to develop a
personalized treatment plan. Early diagnosis and intervention can prevent
complications and help restore your well-being.
Call to Action:
If you're experiencing chronic sinus issues or want expert
advice on how to manage sinus infections, contact a healthcare professional for
a thorough evaluation and personalized care plan.



:max_bytes(150000):strip_icc()/VWH_Illustration_Allergies-vs-Sinus-Infections_Illustrator_Sydney-Saporito_Final-fd354a1641c34216b3642292fb6ee1f7.jpg)



Comments
Post a Comment